The debate of spinal decompression vs surgery isn’t about which treatment is “better” overall – it’s about which is right for YOUR specific condition.
Understanding the difference between non-surgical spinal decompression vs surgery could save you months of recovery time, thousands of dollars, and potentially unnecessary risk. Let’s break down everything you need to know to make the most informed decision about your spine health.
Conditions Treated
Best Conditions for Spinal Decompression
Non-surgical spinal decompression works exceptionally well for conditions where the disc itself is the primary problem but hasn’t caused severe structural damage or emergency neurological symptoms.
We see outstanding results with:
- Mild to moderate disc herniation: When the disc bulges but hasn’t completely ruptured
- Bulging discs: Early-stage disc problems before severe herniation occurs
- Degenerative disc disease: Age-related wear and tear causing chronic pain
- Sciatica: Nerve pain radiating down the leg from disc pressure
- Chronic low back pain: Persistent discomfort related to disc degeneration
- Mild foraminal stenosis: Narrowing of the spaces where nerves exit the spine
Research by Apfel et al. in Neurological Research found that 71% of patients with herniated discs experienced significant pain reduction with decompression therapy, avoiding surgery entirely.
See more: The Benefits of Spinal Decompression
Conditions That Often Require Surgery
Some situations leave little room for conservative treatment. Surgery becomes necessary when:
- Severe spinal stenosis: Advanced narrowing of the spinal canal creating unbearable symptoms
- Cauda equina syndrome: A medical emergency causing loss of bladder/bowel control
- Massive disc herniations: Complete disc ruptures with severe nerve compression
- Spinal instability: When vertebrae shift dangerously, risking spinal cord injury
- Progressive neurological deficits: Worsening weakness, numbness, or loss of function despite conservative care
These aren’t conditions where we debate decompression therapy vs back surgery – surgery is medically indicated, and delaying it could cause permanent damage.
Conditions Where Either May Work
Interestingly, many conditions fall into a middle ground where both approaches might succeed. This includes sciatica, chronic back pain, mild stenosis, and degenerative disc disease.
In these cases, the general medical consensus follows a “conservative care first” approach. Try non-invasive options for 6-12 weeks, and if symptoms don’t improve significantly, then consider surgery.
Comparing Effectiveness: What Really Works?
Effectiveness of Spinal Decompression
Non-surgical spinal decompression works by creating negative pressure inside your spinal discs. This gentle stretching force helps retract herniated or bulging disc material while drawing nutrients and hydration back into the disc.
Studies show impressive outcomes:
- 71-89% of patients report significant pain reduction (Gose et al., Neurological Research)
- Improved disc height and hydration on follow-up MRI imaging
- Long-term relief when combined with rehabilitation exercises
Decompression excels for chronic, non-urgent cases where the goal is healing the disc itself rather than emergency decompression. It’s particularly effective as an alternative to back surgery for patients who haven’t responded to standard chiropractic care or physical therapy alone.
However, decompression won’t work if you have complete disc rupture, severe instability, or progressive neurological symptoms. It also requires patient commitment – typically 20-30 sessions over 6-8 weeks.
Effectiveness of Spinal Surgery
Surgical procedures like microdiscectomy, laminectomy, or fusion offer high success rates for appropriate candidates. When you have severe nerve compression causing unbearable pain or neurological deficits, surgery often provides faster relief than conservative options.
Success rates vary by procedure:
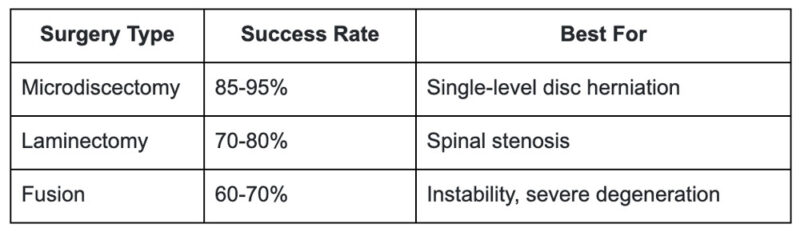
The catch? Surgery addresses the immediate compression but doesn’t fix the underlying disc degeneration. According to research by Parker et al. in Spine Journal, approximately 10-15% of patients experience recurrent symptoms within 5 years, sometimes requiring revision surgery.
Risks & Side Effects
Risks of Spinal Decompression
The beauty of non-surgical spinal decompression lies in its minimal risk profile. Most patients experience:
- Temporary soreness (similar to a workout)
- Occasional muscle spasms during initial sessions
- Fatigue as the body heals
Serious complications are extremely rare. We don’t use decompression if you have fractures, tumors, severe osteoporosis or pregnancy – but beyond these contraindications, it’s remarkably safe.
Risks of Spinal Surgery
Surgery inherently carries more significant risks:
- Infection: Occurs in 1-4% of cases despite sterile protocols
- Nerve damage: Permanent numbness or weakness in 1-2% of patients
- Failed Back Surgery Syndrome (FBSS): Chronic pain persisting or worsening after surgery, affecting 10-40% of patients
- Anesthesia complications: Ranging from minor reactions to serious cardiovascular events
- Scar tissue formation: Can create new sources of pain
- Need for revision surgery: Required in 10-15% of cases within 5-10 years
Recovery Time & Healing Expectations
Recovery After Spinal Decompression
This is where decompression truly shines – zero downtime. You walk in, receive treatment, and walk out the same day. Most patients:
- Return to work immediately (even office jobs)
- Drive themselves to and from appointments
- Continue most daily activities with minor modifications
- Begin exercising within days to weeks
The treatment itself takes 20-30 sessions, but each session lasts only 30-40 minutes. You’re not losing weeks or months of your life to recovery.
Recovery After Surgery
Surgical recovery is a different story entirely. Expect:
- Hospital stay: 1-5 days depending on procedure complexity
- Initial recovery: 2-6 weeks of significant activity restrictions
- Physical therapy: Often required for 3-6 months post-surgery
- Return to work: 6-12 weeks for most desk jobs, longer for physical labor
- Full function: Can take 6-12 months for complete healing
During recovery, you’ll face restrictions on lifting (typically nothing over 5-10 pounds initially), bending, twisting, and prolonged sitting or standing.
What Will This Really Cost You?
Cost of Spinal Decompression
Non-surgical spinal decompression typically costs:
- $100-200 per session without insurance
- 20-30 sessions for complete treatment protocol
- Total out-of-pocket: $2,000-6,000 depending on your insurance coverage
Many insurance plans cover decompression therapy, though coverage varies. Some patients pay entirely out-of-pocket, while others have most costs covered after meeting their deductible.
Cost of Spinal Surgery
Spine surgery costs significantly more:
- Surgeon fees: $5,000-15,000
- Hospital charges: $15,000-50,000
- Anesthesia: $1,000-5,000
- Imaging and tests: $2,000-5,000
- Post-operative physical therapy: $2,000-6,000 over several months
Total cost: $25,000-100,000+ depending on procedure complexity. While insurance typically covers most surgical costs, your deductible and co-insurance can still leave you with $3,000-10,000+ in out-of-pocket expenses.
Spinal Decompression vs Surgery: Which Should You Choose?
Now for the million-dollar question – which path is right for you?
When to Choose Spinal Decompression
Consider non-surgical spinal decompression if you:
- Want a completely non-invasive approach without surgical risks
- Can’t afford significant time off work for recovery
- Prefer drug-free solutions for pain management
- Hope to avoid surgery or delay it until absolutely necessary
- Have mild to moderate disc problems without emergency symptoms
- Want to address the root cause through structural correction and healing
As a chiropractor New City, NY patients trust for complex spine cases, I always recommend starting here unless surgery is medically urgent.
Surgery May Be Necessary If You Have:
Don’t delay surgery if you experience:
- Loss of bladder or bowel control (cauda equina syndrome)
- Progressive weakness in legs despite conservative care
- Severe, unrelenting pain that prevents sleep or basic function
- Major spinal instability shown on imaging
- Documented failure of 6-12 weeks of appropriate conservative care
In these situations, when to choose spine surgery becomes clear – the benefits far outweigh the risks.
Your Personal Decision Checklist
Consider these factors:
- Symptom severity: Emergency symptoms = surgery; chronic pain = decompression first
- MRI/imaging results: Degree of herniation and nerve compression
- Lifestyle demands: Can you take 3 months off work, or do you need minimal downtime?
- Financial situation: Insurance coverage and out-of-pocket affordability
- Personal preference: Conservative vs. surgical intervention philosophy
- Previous treatment response: What have you tried, and what were the results?
Making the Right Choice for Your Spine
Here’s the bottom line on spinal decompression vs surgery: Surgery should be your last resort unless you have medically urgent symptoms. The research strongly supports a “conservative care first” approach.
Most major medical organizations, including the American College of Physicians, recommend exhausting non-surgical options before considering surgery for back pain. This means appropriate chiropractic care, physical therapy, and when indicated, spinal decompression therapy.
However – and this is crucial – proper diagnosis through advanced imaging is essential. We never guess. You need current MRI results to determine which treatment path makes sense.
At DeCarlo Chiropractic, we’ve helped countless patients avoid unnecessary surgery through evidence-based decompression protocols combined with structural correction and rehabilitation. But we also know when to refer patients for surgical consultation because their condition demands it.
Ready to explore whether decompression could help you avoid surgery? Schedule your comprehensive evaluation at our New City office. We’ll review your imaging, assess your specific condition, and give you honest answers about your best treatment options.
Frequently Asked Questions
Is spinal decompression safe?
Yes, extremely safe. Serious complications are exceptionally rare. The treatment is FDA-cleared and has been used successfully for decades.
Does spinal decompression hurt?
Not at all. Most patients find it relaxing, even pleasant. You might feel a gentle stretching sensation, but it shouldn’t cause pain.
Can decompression replace surgery?
For appropriate candidates – yes. Studies show 71-89% of patients with disc herniations avoid surgery through decompression therapy.
What happens if I avoid surgery too long?
If you have progressive neurological symptoms, delaying surgery could result in permanent nerve damage. However, for chronic pain without neurological deficits, conservative care first is appropriate.
How do I know if decompression will work for me?
Schedule a consultation with a qualified provider who reviews your MRI and performs a thorough examination. We can typically predict your likelihood of success based on your specific findings.

